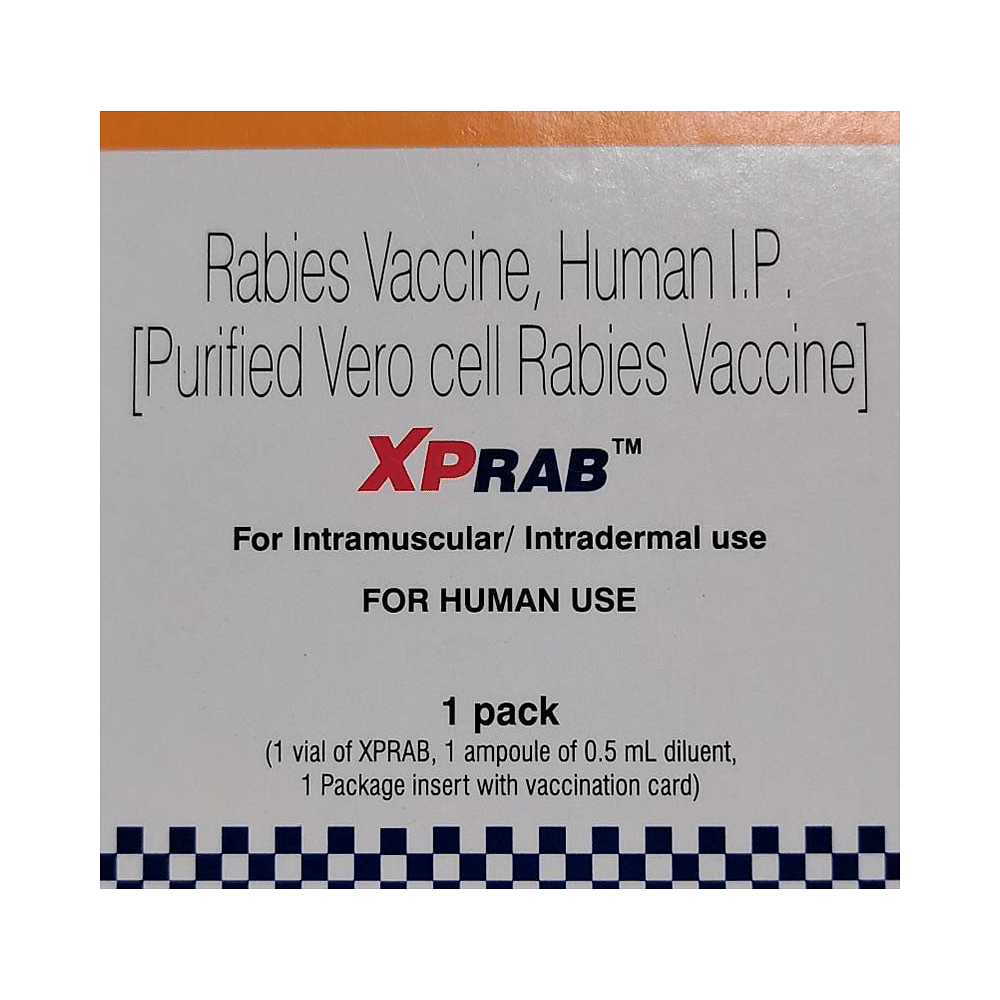
Xprab Vaccine
Manufacturer
Sun Pharmaceutical Industries Ltd
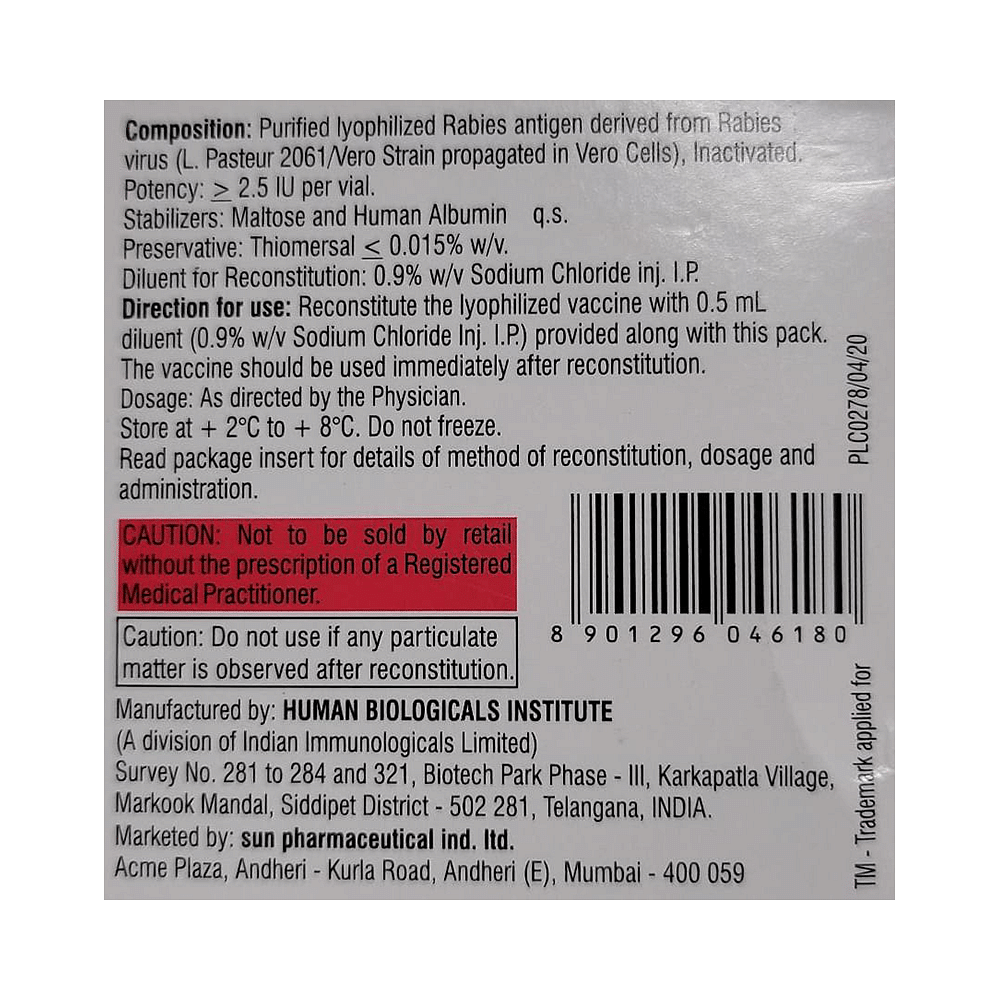
Salt Composition
Rabies vaccine, Human (150IU)
Key Information
Short Description
Xprab Vaccine is given to people who are at higher risk of coming in contact with rabies, such as veterinarians, and to people after an animal bite if the animal could have rabies.
Dosage Form
Injection
Introduction
Xprab Vaccine is given by injection by a doctor or nurse. It is administered post thorough washing of all bite wounds as early as possible. The sooner treatment is begun after exposure, the better. Post-exposure anti-rabies vaccination should always include administration of both Immunoglobulin and vaccine, with the exception of persons who have previously received complete vaccination regimens. It is very important to complete the course of the vaccine to prevent this fatal disease.
Directions for Use
Your doctor or nurse will give you this medicine. Kindly do not self-administer.
Safety Information
Side Effects
Pain Joint pain Vaccination site redness as well as swelling
Alcohol Warning
It is not known whether it is safe to consume alcohol with Xprab Vaccine. Please consult your doctor.
Breastfeeding Warning
Xprab Vaccine is probably safe to use during breastfeeding. Limited human data suggests that the drug does not represent any significant risk to the baby.
Pregnancy Warning
Xprab Vaccine is generally considered safe to use during pregnancy. Animal studies have shown low or no adverse effects to the developing baby; however, there are limited human studies.
Interacting Medicines
Mycophenolate mofetil Azathioprine Cyclophosphamide Mercaptopurine
How it works
Xprab Vaccine is an inactivated vaccine. It helps develop immunity by forming antibodies which are proteins that protect against infection caused by viruses.
Quick Tips
Xprab Vaccine helps prevent rabies. It is given as an injection into the muscle of the upper arm. If you are at risk of being bitten, the vaccine is given as a course of three injections on 0, 3, and 7 days. A booster dose is needed one year after completing this course. You may experience headaches or fatigue. Inform your doctor who may prescribe you a suitable painkiller to give you relief. Never self-medicate.
Frequently asked questions
How does rabies spread?
Rabies is caused by a virus that spreads through the saliva of infected animals. People usually become infected with rabies after a bite from an infected animal. However, contact with the saliva of an infected animal (alive or dead) can also lead to infection if there are breaks in the skin or if the saliva gets into the eyes, nose, or mouth.
Is rabies preventable?
Yes, rabies is 100% preventable. Proper wound management and simultaneous administration of Xprab Vaccine combined with rabies immunoglobulin (RIG) are considered highly effective in preventing rabies, even after high-risk exposure.
What are the symptoms of rabies?
The rabies virus attacks the nervous system. The first signs of rabies mimic a flu-like illness. These include fever, headache and general discomfort. Within days, the disease progresses to anxiety, confusion, agitation, abnormal behavior, delirium, and hallucinations.
Who should get this vaccine?
Rabies vaccine is recommended for individuals in high-risk occupational groups, such as veterinarians, animal handlers, rabies researchers, and laboratory workers. International travelers who may be exposed to animals in areas with high dog rabies rates should also consider vaccination.
Can a pregnant woman receive Xprab Vaccine if exposed to rabies?
Yes, Xprab Vaccine can be taken by pregnant women. There have been no reported fetal abnormalities associated with the use of Xprab Vaccine in pregnancy. The doctor may also suggest pre-exposure vaccination against rabies if the risk of exposure is high.
What are the side effects of Xprab Vaccine?
Most side effects of Xprab Vaccine are mild, such as pain or redness at the injection site. Moderate problems, including hives, joint pain and fever, may occur in a small percentage (6%) of patients who receive booster doses.
Who should not receive Xprab Vaccine?
Xprab Vaccine is not routinely recommended for the general population. It should not be used if a person has a severe illness. If you have any concerns, consult your doctor.


