Esmocam-LS Capsule SR
Manufacturer
Hilbert Healthcare
Salt Composition
Levosulpiride (75mg) + Esomeprazole (40mg)
Key Information
Short Description
Esmocam-LS Capsule SR is a prescription medicine used to treat gastroesophageal reflux disease (acid reflux) by relieving symptoms such as heartburn, stomach pain, or irritation.
Dosage Form
Capsule SR
Introduction
Esmocam-LS Capsule SR is a prescription medicine used in the treatment of gastroesophageal reflux disease (acid reflux). It works by relieving the symptoms such as heartburn, stomach pain, or irritation. It also neutralizes the acid production in the stomach to prevent discomfort.
Directions for Use
Take this medicine in the dose and duration as advised by your doctor. Swallow it as a whole. Do not chew, crush or break it. Esmocam-LS Capsule SR is to be taken empty stomach.
How it works
Esmocam-LS Capsule SR is a combination of two medicines: Levosulpiride and Esomeprazole.
Quick Tips
Do not consume alcohol while taking Esmocam-LS Capsule SR as it can increase the risk of stomach damage. Long-term use may cause weak or broken bones. Take adequate intake of dietary calcium and vitamin D or their supplements. Do not take Esmocam-LS Capsule SR for longer than prescribed.
Related Medicines

Esofag-L Capsule SR
Sompraz L Capsule
Esogress-L Capsule

Isozole-L Capsule SR

Esomac L Capsule SR

Easemo-L Capsule SR
Esmonova-L Capsule SR
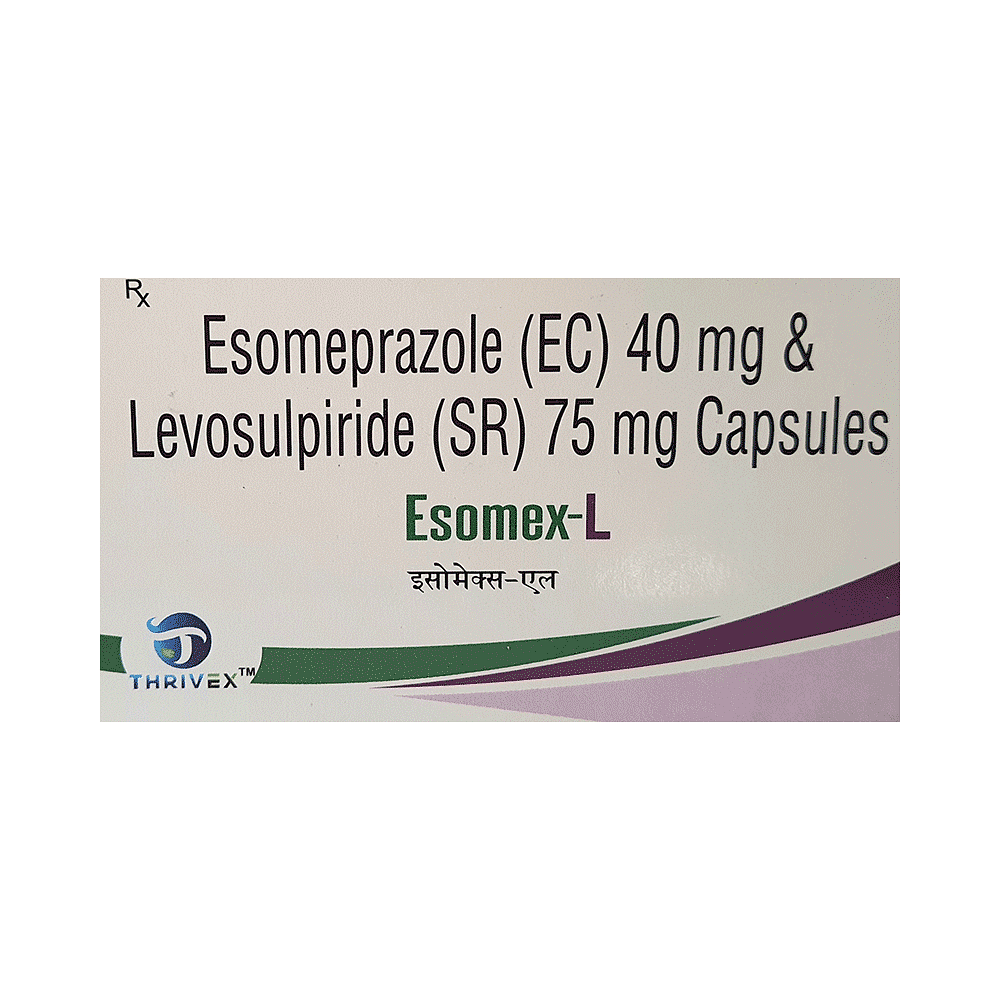
Esomex-L Capsule SR
Esogic LS 75mg/40mg Capsule SR
Esjole L 75mg/40mg Capsule SR
Frequently asked questions
What are the instructions for storage and disposal of Esmocam-LS Capsule SR?
Keep this medicine in its original container or pack it came in, tightly closed. Store it according to the instructions on the label or packaging. Do not dispose of this medication down the drain; it can be harmful to the environment. Make sure it is not accessible by pets, children, or other people.
What is the best time to take Esmocam-LS Capsule SR?
Take Esmocam-LS Capsule SR exactly as directed by your healthcare provider. It's best to take one capsule daily on an empty stomach.
What are the contraindications associated with the use of Esmocam-LS Capsule SR?
The use of Esmocam-LS Capsule SR should be avoided in patients with known allergies to any component or excipients of this medicine.
Can the use of Esmocam-LS Capsule SR cause dizziness?
Yes, some patients may experience dizziness (feeling faint, weak, unsteady, or lightheaded) after taking Esmocam-LS Capsule SR. If you feel dizzy, it's best to rest and resume once you are feeling better.
Does the use of Esmocam-LS Capsule SR lead to increased risk of fractures?
Several studies in adults suggest that treatment with Esmocam-LS Capsule SR may be associated with an increased risk for osteoporosis-related fractures of the hip, wrist, or spine. The risk was higher in patients who received high doses, defined as multiple daily doses over time, and those undergoing long-term therapy (1 year or longer).


